Overview
Spectra Optia
Apheresis System
Cell Collections
Comprehensive cell collection solutions
Red Blood Cell Exchange
Therapeutic Apheresis Red Blood Cell Exchange
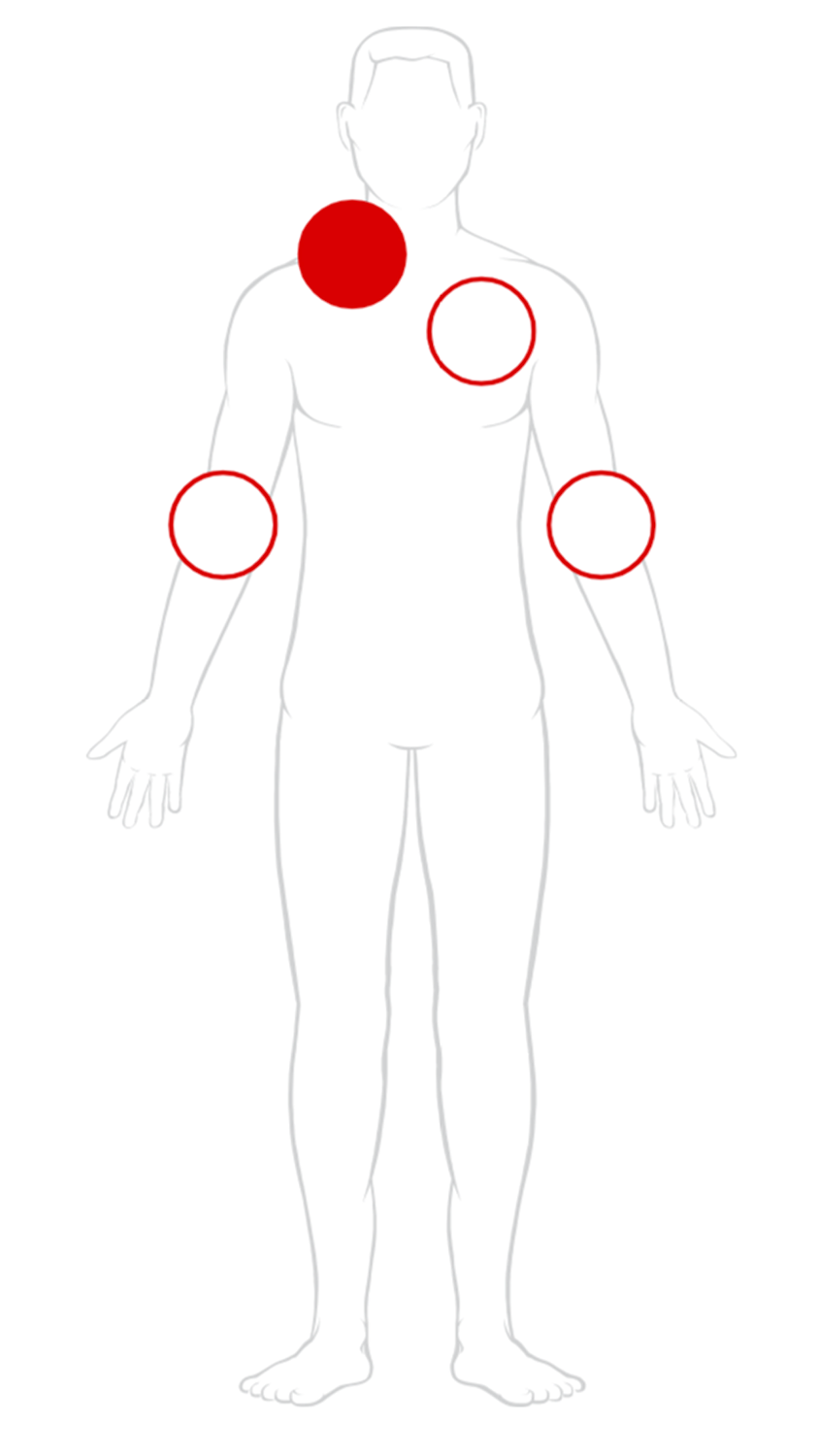
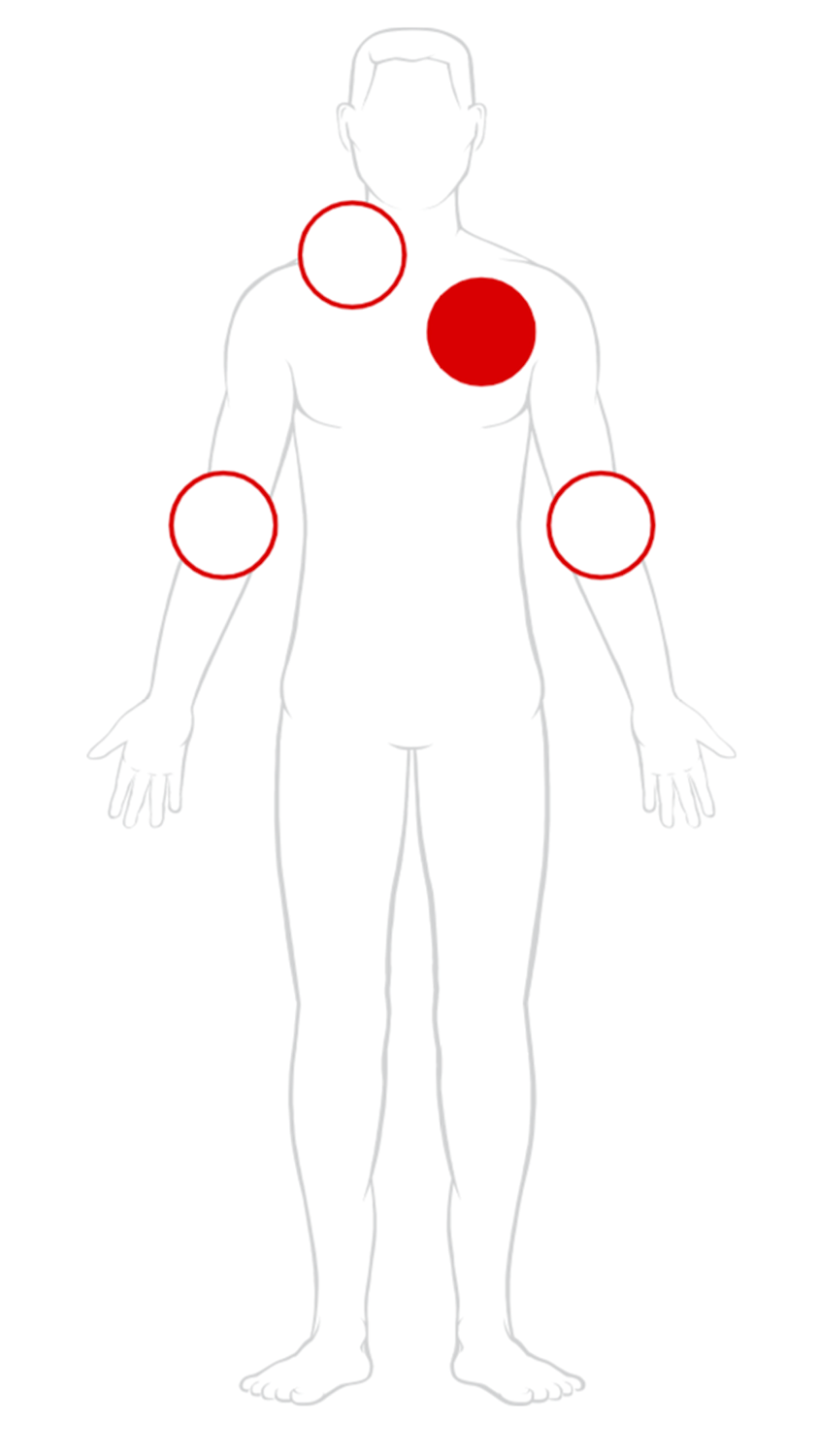
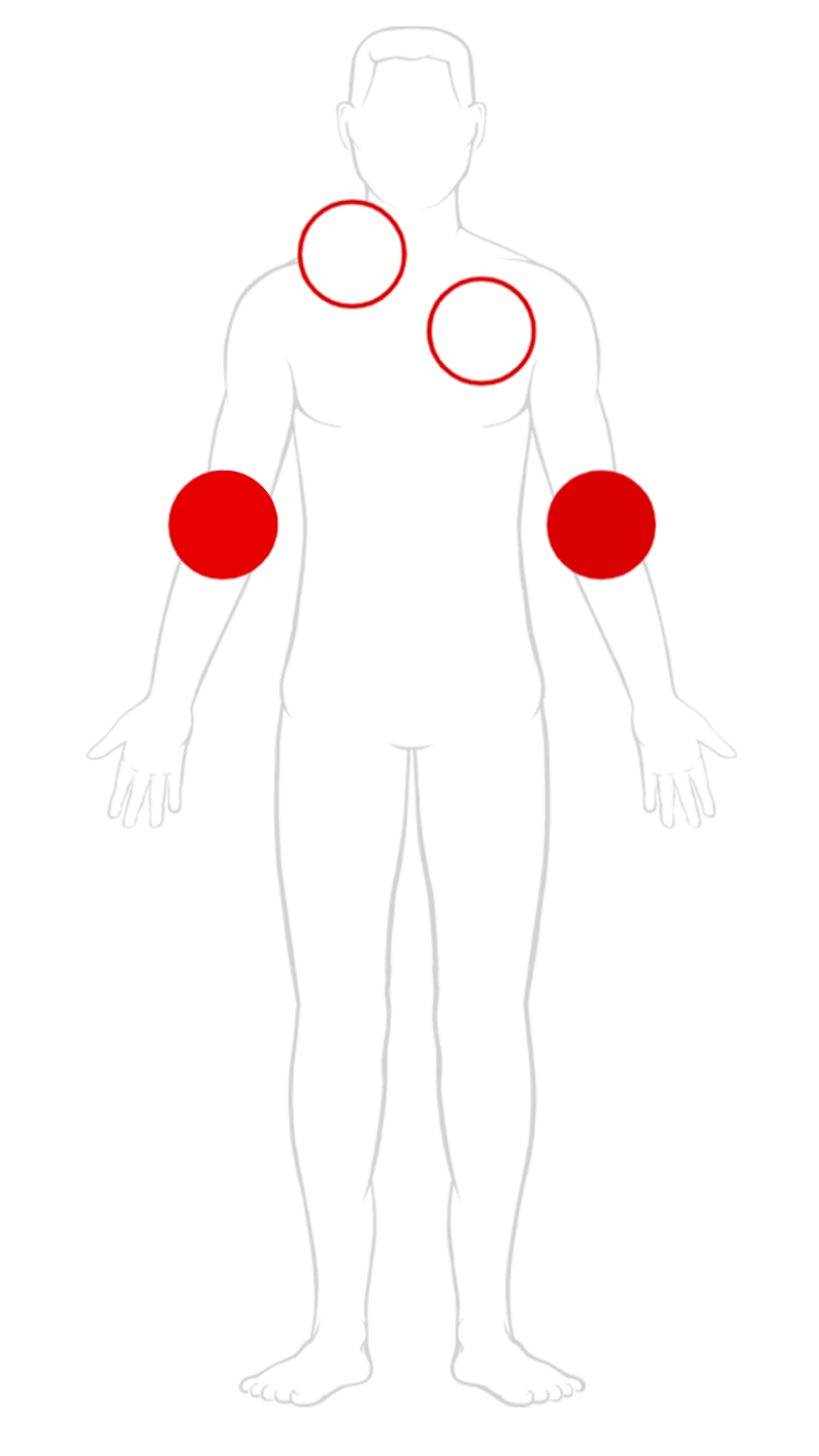
Vascular Access
Your resource for optimizing vascular access for each and every patient
Sickle Cell Disease
Transfusion Therapy for Sickle Cell Disease
See all